Hundreds of times, in waiting rooms outside Intensive Care Units I have looked into the eyes of sons and daughters, spouses and partners of patients, held their hands and said, “We did all we could. I am so sorry for your loss.”
When Saagar died, no one looked into my eyes and said that to me. They had not done all they could for him. The hospital carried out a sham investigation, a futile exercise in ‘being seen’ to be doing the right thing.
The GMC found everything to be hunky dory. The doctors ‘looking after’ Saagar had done their jobs to perfection. Just too bad the patient was dead. They did not deem Saagar’s case worthy of an investigation. GMC’s role in its own words:
“We work to protect patient safety and support medical education and practice across the UK.”
The Coroner’s report shone some light on the holes in Saagar’s care. It clearly pointed out the things that South London and Maudsley (SLaM) Hospital got wrong.
- There was a general failure to identify the diagnosis on the discharge summary from the Home Treatment Team to the GP.
- There was a general failure to communicate thoroughly enough with the parents about the relapse symptoms, what to watch out for and where to go for help in the future.
Last June, I wrote to the CEO of SLaM, requesting an update on the changes that had been made in his organisation in response to the Coroner’s findings above. He said someone would get back to me and I heard nothing. This June, I sent him a reminder and again he said someone would get back to me and I am still waiting.
What are my rights as a parent? Is this too much to ask?
What were Saagar’s rights as a young man with a mental illness?
Are our lives not as important as anyone else’s? Black or white or brown? With Cancer or Diabetes? Or Bipolar Disorder?
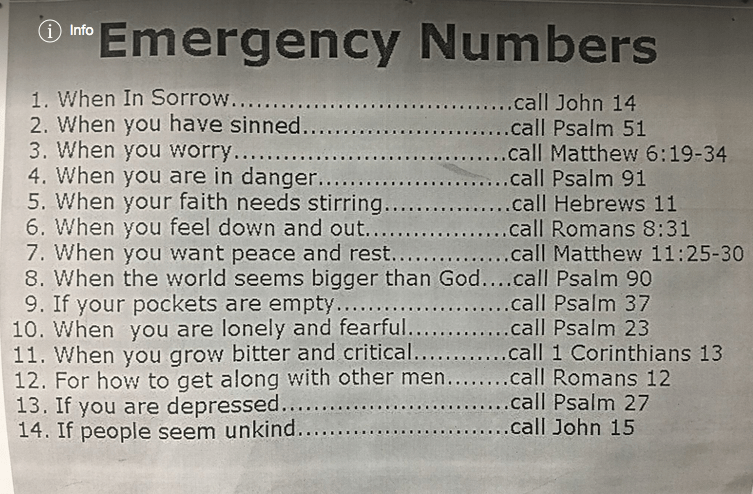
Everyone deserves to be heard and seen. With respect.
It’s not charity. It’s a human rights issue.
Ref: Learning from deaths: Guidance for NHS trusts on working with bereaved families and carers