When our GP heard of Saagar’s death, the first phone call he made was to the Medical Defence Union and they advised him not to call us. Despite having known us for more than 7 years and seeing Saagar every 2 weeks with us for the last few months of his life, he did not call us on his death.
A qualitative study of GPs’ experiences of dealing with parents bereaved by suicide by Emily Foggin et al was published last month in the British Journal of General Practise.
It acknowledged that bereavement by suicide is a risk factor for suicide but the needs of those bereaved by suicide have not been addressed and little is known about how GPs support these patients, and how they deal with this aspect of their work. 13 GPs in the UK were interviewed in a semi-structured format. It explored experiences of dealing with suicide and bereavement.
GPs disclosed low confidence in dealing with suicide and an unpreparedness to face parents bereaved by suicide. Some GPs described guilt surrounding the suicide, and a reluctance to initiate contact with the bereaved parents. GPs talked of their duty to care for the bereaved patients, but admitted difficulties in knowing what to do, particularly in the perceived absence of other services. GPs reflected on the impact of the suicide on themselves and described a lack of support or supervision.
It concluded that GPs need to feel confident and competent to support parents bereaved by suicide. Although this may be facilitated through training initiatives, and accessible services to refer parents to, GPs also require formal support and supervision, particularly around significant events such as suicide. Results from this qualitative study have informed the development of evidence-based suicide bereavement training for health professionals.
Ref : http://bjgp.org/content/early/2016/08/15/bjgp16X686605
This evening a vigil was held by SOBS (Survivors Of Bereavement by Suicide) at Hyde Park to remember those lost through suicide. Some of the people there had lost a brother 25 years ago or a sister 5 years ago or a friend 1 year ago and so on. Some of the families had not been able to speak about it for many years. Others had kept quiet as they were not sure if anyone would understand. But in that space, we sat together on the brownish-green grass with the pictures of our loved ones and lit candles in their memory and we opened our hearts. For about 2 hours we claimed that space and made it our own knowing full well that we are being listened to and perfectly well understood. What a rare gift that is!
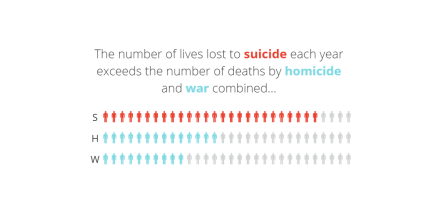
When it comes to suicide, post-vention is pre-vention.
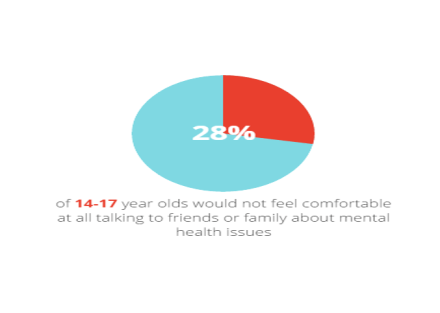
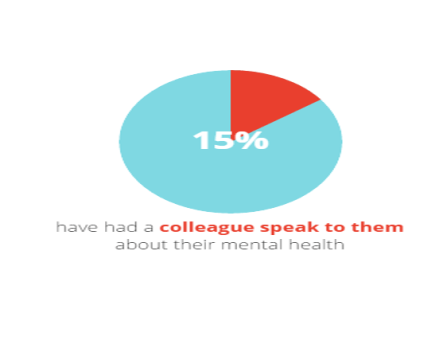
 A survey of 500 people revealed that a third of people didn’t feel comfortable at all talking to someone at work about mental health related issues and only 15% have had a colleague speak to them about their mental health.
A survey of 500 people revealed that a third of people didn’t feel comfortable at all talking to someone at work about mental health related issues and only 15% have had a colleague speak to them about their mental health.