Sunday lunch at the start of autumn on a warm day of blue skies and a warm sun, sitting under a wise old carob tree with supported branches and multiple dried brown beans hanging from a wide umbrella of dark green leaves with friends and strangers making introductions followed by conversations, smiles and laughter, references to this and that, occupations, travels and hobbies, daughters and mothers, food and wine, so on and so forth …. as if straight out of a film set infused with a sweet subtle smell of eucalyptus.
All of it completely meaningless, empty, futile, feckless, inane and pointless. Words, words and more words! Exhausting! I had to get up and walk away with my i-pad and take pictures of something. Anything.
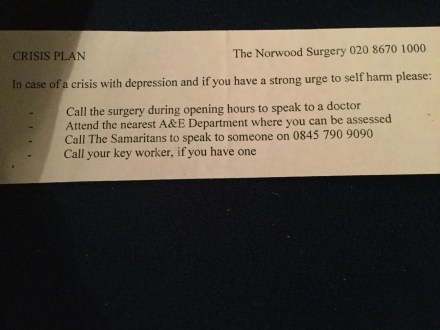
In 2 weeks time he will be dead. Around this time 2 years ago he was scoring max on his depression scores and he gave it in writing to his GP in the form of a PHQ-9 form but got no help. No escalation of care. No attention. No mention of ‘suicide’ to us and yet holding a firm belief that a safety plan was in place. Sent home with the suggestion, “It will get better. Give it time. Rome was not built in one day” and a piece of paper.
It was early autumn then and it is early autumn now.
I lived in what I thought was our world then.
I live in a world of my own now. It sort of overlaps with this one in places but most of this one is irrelevant to me.


