Vikram Patel is a psychiatrist and a Professor of Global Health who works tirelessly to improve the mental health of people living in low and middle income countries like India and Ethiopia.
His recent research has found that all countries are ‘developing’ countries when you look at the low proportion of the health-budget they spend on mental health. Some wealthy countries may have better systems of care for maternal and child health but overall, mental health remains universally, at the end of the queue.

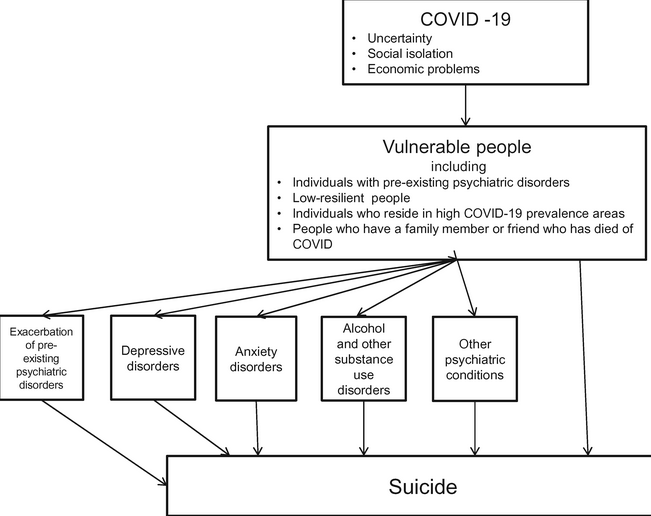
At present, COVID has overtaken all other agendas. However, now more than ever before, there is a recognition of the two-way relationship between poverty and mental ill-health. This may be a historic opportunity to get this right.
The relationship between poverty and mental ill-health is a complex one. How can we distinguish a normal response to poverty from a disease process? Poverty can increase the risk of poor mental health via multiple pathways, for example, poor physical health, high levels of noise pollution, violent neighbourhoods, insecurity and humiliation.
Can an increase in income improve mental health? Yes. It can but it needs to be sustained.
The fact that having a mental illness may induce poverty is less well recognised. It may affect one’s education and hence, employment opportunities. In low and medium income countries, health care is paid for by people. Due to the length of time it takes to find an effective treatment, much effort and money is wasted in doctor-shopping. Depression is inequitably distributed in society but not recognised as such because wealthy individuals also get it. We accept that long term expensive therapies cannot be delivered to the poor, so what’s the point in studying them?
After nearly a year of job-losses, the number of people below the bread-line all over the world will increase by tens of millions. In India alone, the gains made in economic growth over the last decade are predicted to be wiped out this year. The historically disadvantaged will fare worse, suffer more.
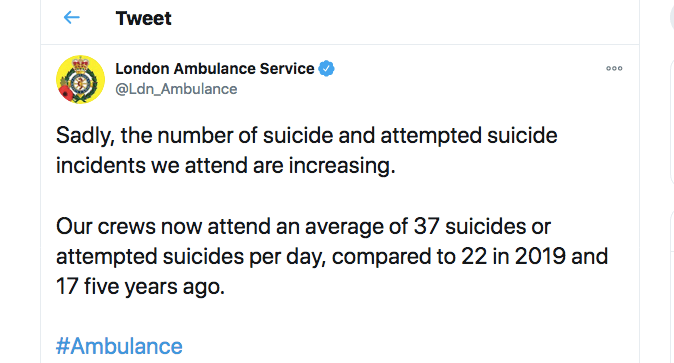
We can expect a surge in mental health problems like we did after the 2008 global financial crisis, mainly led by suicide and drug misuse. Sir Angus S Deaton, a Nobel prize winning economist wrote extensively about these deaths of despair. Economists and global health experts warn that this one will possibly be far worse.
In India, while the state is spending all its energies on the pandemic, livelihood-based organisations are finding very poor mental health in their members. Taking a broad, multidisciplinary approach to depression and anxiety rather than viewing it through the lens of a medical specialty is the need of the hour. Policies all over the world need to de-medicalise the emphasis on specialists and empower front-line providers and communities to enable them to foresee, identify and address this problem.
The bi-directional relationship between mental health and finances means that appropriate mental health interventions can improve finances. Can we persuade policy-makers world-wide to listen to global health experts and economists, look at this fast-approaching avalanche and steer policies to protect those who are being and will be hit by it?
Talk: Poverty and Depression (https://voxdev.org/topic/health-education/poverty-and-depression-how-improving-mental-health-can-help-economic-wellbeing) – this talk was available till last night but has since disappeared.
Research Papers:
- Angus Deaton on the Financial crisis and the well-being of Americans (June 2011):
https://www.nber.org/papers/w17128
2. Vikram Patel on Causal evidence and mechanisms of Poverty, Depression and Anxiety (May 2020):